Why Suppress Airborne Virus Transmission
The evidence base below, based on research by scientists and engineers, outlines the case for action. The Covid-19 Safety Pledge NZ provides scientific evidence and references throughout, including early signals from pre-print findings where relevant to our rapidly improving understanding of the virus.
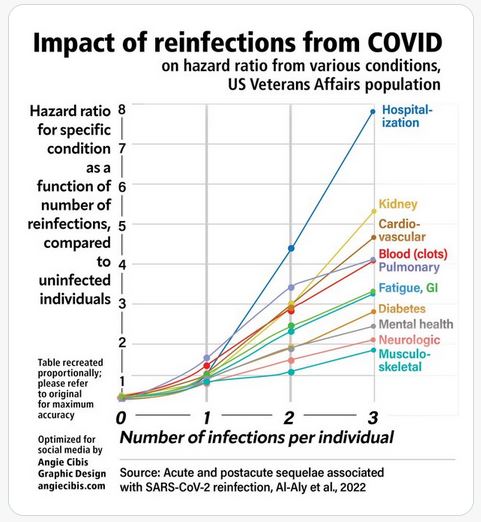
Avoid virus transmission to avoid workforce disability.
The incidence of long COVID in adult survivors of an acute SARS-CoV-2 infection is approximately 11%.
Of those afflicted, 26% have difficulty with day-to-day activities.
The majority of long COVID cases occur after mild or asymptomatic acute infection. Children can spread SARS-CoV-2 infections and can also develop long-term neurological, endocrine (type I diabetes), and immunological sequelae.
Immunological hypofunction (following COVID) is exemplified by the recent large outbreaks of respiratory syncytial virus and streptococcal infections. source
The most productive labour force is affected.
Prevent virus transmission to improve business performance.
Protecting your workforce and customers with clean air is an investment in your organisation and your people:
- reduce transmission by 74% with mechanical ventilation.
- reduce short term sick leave by up to 35% by improving ventilation from 12 to 24 L/s/person.
- reduce team sickness by 50% with universal masking.
- improve productivity by up to 8% by increasing ventilation from 10 to 20 L/s/person.
- control all respiratory illnesses with clean air
- show your customers your business or venue is COVID safe.
- display the Pledge and improve trust in your business.
“An estimated one in 10 infections results in post Covid condition suggesting that hundreds of millions of people will need longer term care”. WHO – 27 April 2023
link to video source
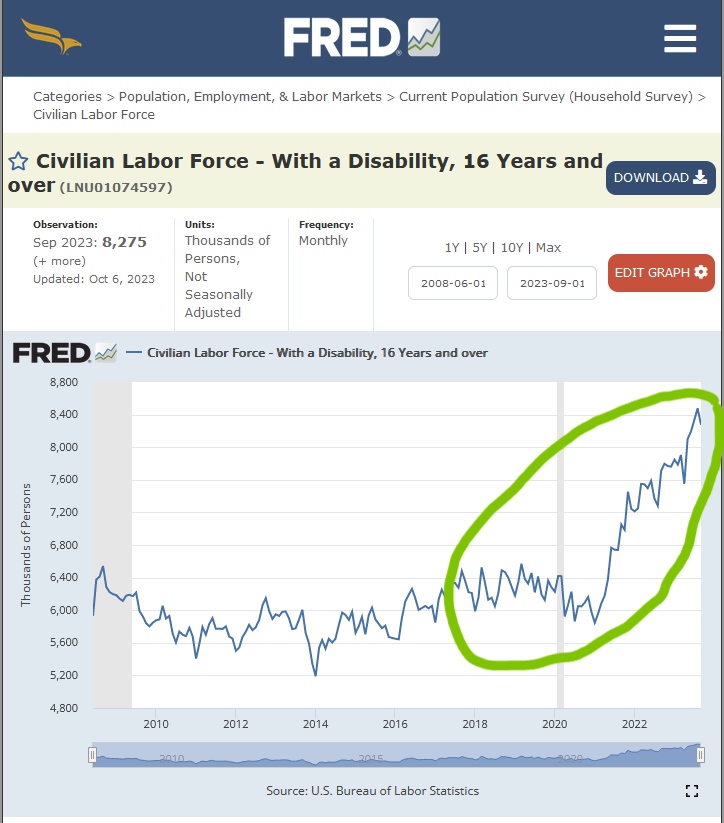
Avoiding COVID avoids worker shortages due to Long-COVID
Link to original CDC paper/presentation.
New Zealand used to lead the world on COVID safety, we can do so again.
Contents include:
- Know the risk of airborne COVID-19 spread.
- How laboratory workers protect themselves
- The ongoing impact of the virus and variants in Aotearoa.
- Safer locations can make a difference.
- Vaccination reduces severe outcomes.
- Ventilation reduces risk of COVID-19 spread.
- Mask use reduces risk of COVID-19 spread.
- Virus transmission control is possible
Know the risk of airborne COVID-19 spread
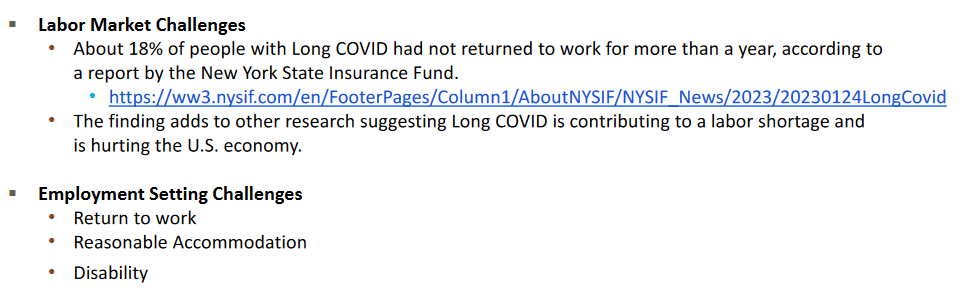
- Elevated CO2 levels relate to higher risk, eg. CO2 calculated at 2517ppm during a two and a half hour choir practice lead to 53/61 people getting COVID-19.
- Risk is highest with crowding and stuffy air because COVID-19 is airborne.
- One elevator ride with someone with COVID may be enough to become infected.
- Nearly all COVID-19 spread is indoors with some exceptions.
- Airborne transmission is 1000 times more likely than surface transmission.
- Up to half of people with Omicron have no symptoms.
- Virus is spread by breathing and more so with talking and especially with singing/shouting and exercising.
- Airborne virus survives for hours indoors, so unless virus is removed, clouds of virus can build up indoors and spread.
- Risk is highly related to duration of exposure.
- COVID-19 is frequently spread by people before they get symptoms.
How laboratory workers protect themselves
Laboratory workers protect themselves with strict protocols and filtered clean indoor air because SARS-CoV-2 (the virus that causes COVID-19) is a Biosafety/Biohazard Level 3 (BSL-3) contagion.
BSL-3 Safety Requirements:
- Individuals wear PPE and respirators.
- Double self-closing and locking doors with restricted or controlled access at all times.
BSL-3 infections include: SARS-CoV-2 (COVID-19), Anthrax, West Nile Fever and Tuberculosis.
The ongoing impact of the virus and variants in Aotearoa/New Zealand
It’s unclear what is going to stop exponential growth of multiple variants.
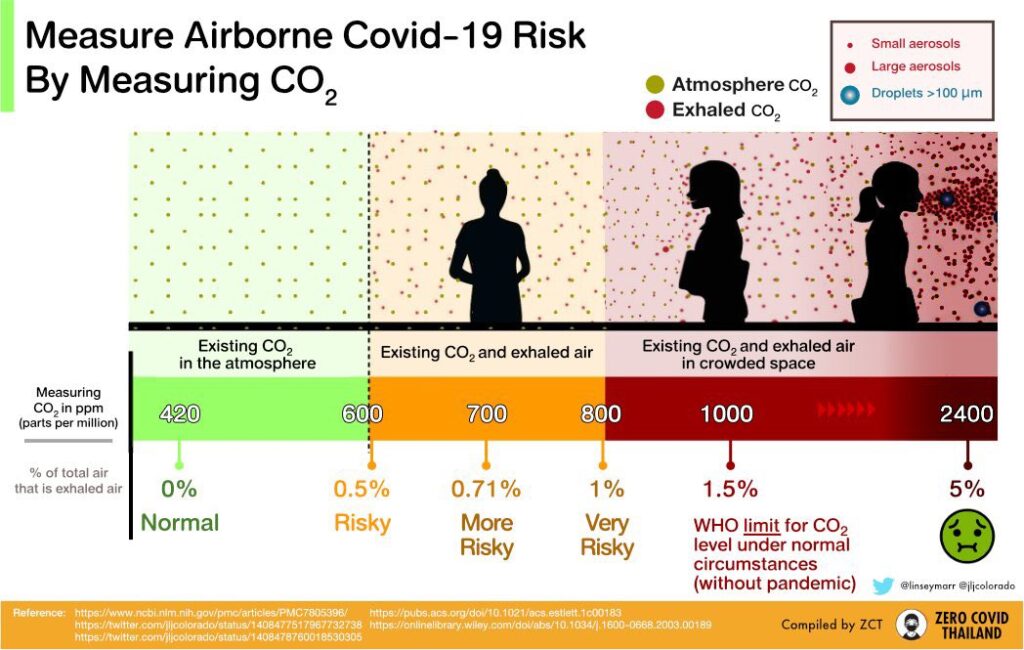
- Each infection/re-infection increases the chance of long periods off work.
- Vaccine effectiveness is temporary – as low as 24% at 120-179 days leading to breakthrough and repeat infections.
- New variants causing new infections and reinfections means that we cannot rely on herd immunity.
- Many COVID-19 infections may result in Long-COVID and some people are disabled for long periods including approximately 12-16% of children with each infection.
- Specific medical conditions increase in frequency following infection and become more likely with each infection (chart below).
COVID-19 transmission has now become widespread within New Zealand, with more than 3 million people estimated to have had the virus. However this only makes it more important that we continue to take action against the virus.

Safer locations can make a difference
Virus spread is heavily dependent on super-spreader events. It appears that 4% of people may cause 80% of transmission. While we cannot identify these people, we can identify and protect superspreading locations where intervention is super-effective in curbing transmission.
Lived experience of public health in New Zealand indicates these locations:
- Offices and workplaces.
- Schools*.
- Hospitals**
- Aged Residential Care.
- Early childhood education centres.
- Places of worship.
- Funerals.
- Gymnasiums.
- Marae.
- Restaurants, cafes.
- Shared living facilities.
- Bars and nightclubs.
- Conferences.
- Temporary housing.
- Corrections facilities.
- Disability care services.
- Transport (bus, train, car, ships and aircraft).
*Schools drive community infection, and school opening/closing synchronise with community infection. This correlation was missed early on because many children have no symptoms. In USA 70% of household COVID-19 spread from a child (underestimate, relied on symptoms to detect infection).
**Hospital acquired COVID-19 appears particularly lethal. Figures from Australia indicate 60 to100 times greater mortality when compared with community acquired COVID-19.
Where these locations and organisations have, at least clean air, the risk of COVID-19 can be significantly reduced.
Vaccination reduces severe outcomes
COVID-19 vaccination and boosters in 2023 are still helping avoid severe outcomes and possibly reducing Long-COVID.
However clean air actions are needed because vaccination cannot entirely prevent infection or transmission. At 20 weeks following vaccination nearly all will be able to catch and transmit Omicron (Page5, Figure1).
New variants are likely to keep on emerging globally, and the impact of vaccination on these will be variable.
Clean air reduces risk of COVID-19 spread
Why does clean air matter?
Clean air dilutes and takes away contaminated air. Clean indoor air works on any variant and any airborne disease. Increasing and enhancing ventilation with clean air makes indoor places more like the outdoors, significantly reducing the risk of COVID-19 transmission and it doesn’t take away anyone’s freedom. The closer indoor CO2 levels are to outdoor CO2 levels of 420ppm the lower the risk.
Minister of Health, Dr Ayesha Verrall (14 July 2022).
How effective is clean air ?
In addition to improved productivity and reduced short-term illness, studies show that clean air ventilation at 20L/sec/person can reduce COVID-19 risk by 80% (approx = 5-6 air changes per hour with 1.25m distancing).
- When air was replaced 2.4 times an hour by the ventilation system, infections were lowered by 40 per cent
- When air was replaced four times an hour, infections were lowered by 66.8 per cent
- When air was replaced six times an hour, infections were lowered by 82.5 per cent
For building owners and managers ventilation is your first priority.
See ‘how-to’ at clean air ventilation methods.
Mask use reduces risk of COVID-19 spread
N95, or KN95 or KF94 masks can stop you breathing in approx. 94+% of viruses .
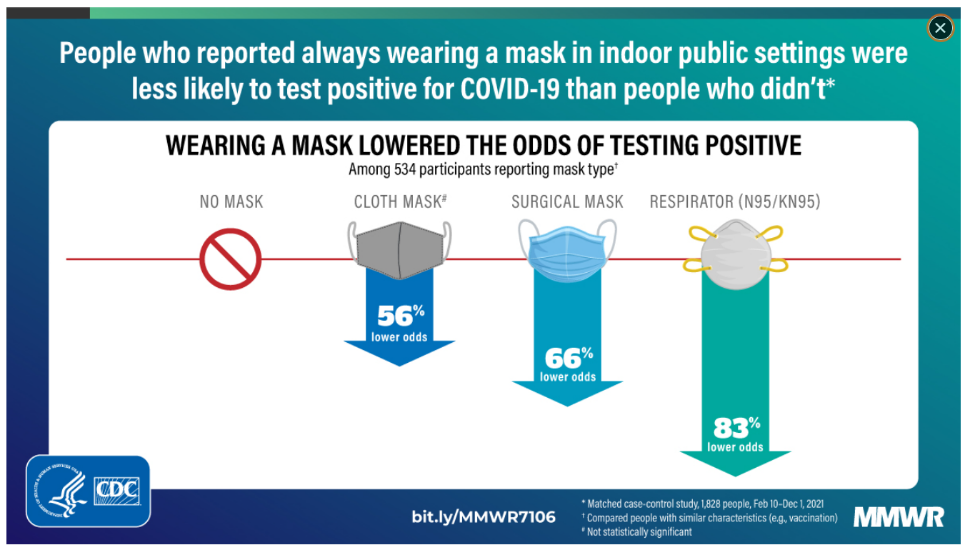
Masking offers triple protection. It protects the wearer, people nearby as well as others indoors in the same area. Masks work on any variant.
The cost of masks
N95 masks can theoretically be used 200 days in total and are approximately NZ$1.80 each. They can be used for a standard working week (up to 40 hours ,5 x 8hr ) then re-used after resting for 3 days (provided the mask still fits well). This means the average cost is 9 cents/day.
Surgical/medical masks cost approximately 20 cents each, and can be washed up to 10 times. If one mask is used per day this is approximately 2 cents/day.
Virus transmission control is possible
This example and this example and many others demonstrate the value of clean indoor air.
Clean indoor air and mask use can suppress virus transmission.
