Methods to Suppress Airborne Virus Transmission
“People see the pandemic and think the solution has to be medical when the solution is actually engineering.” – Prof Christina Pagel.
Contents include:
- Choose appropriate ventilation.*
- Find and remove stagnant air.
- Match ventilation to occupancy.
- Mask to avoid close range infection.
*The following guidance is general rather than specific engineering advice.
Choose appropriate ventilation
Increase natural ventilation
- If feasible open all; windows, doors and vents, aim for crossflow if possible. Crossflow is approximately 10x more effective than single sided openings.
- Pro – Ultimate DIY, lowest cost option, effect can be excellent eg. 16-25 air changes per hour (ACH) in moderate conditions (ref required).
- Con – Potentially unreliable, dependent on human vigilance. Not always feasible, maybe noisy or un-private and room pre-heat or intermittant room purging may be required in winter. Care required to avoid directing contaminated air towards sub-groups of occupants eg. kitchen staff in a cafe may be at increased risk if infective air goes through the kitchen.
Improve mechanical ventilation (HVAC)
- Increase fresh air, eliminate recirculation, improve filters. Adopt ASHRAE 2023 Control of Infectious Aerosols recommendation (below). Eg. 20 L/sec/person clean air in each office room.
- Pro – Reliable, excellent air mixing, virus/particle dilution and extraction.
- Con – Technician required, may increase thermal load.
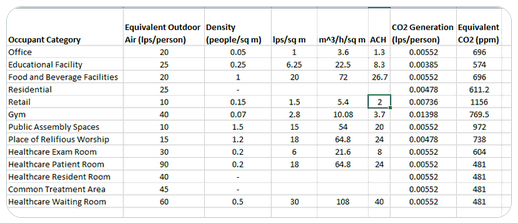
ASHRAE 2023 Control of Infectious Aerosols Initial Public Recommendations.
Interpretation by engineer Joey Fox
Clean and mix the air
- Air cleaner +/- fan. Air movement can mitigate stagnant air.
- Pro – DIY, can be very effective, air cleaners can be less than NZD$200 each, make your own is possible. Air cleaner units can add additional clean air changes to bring clean air equivalent up to 20L/sec/person. Engineering background. University of Melbourne air cleaner guide.
- Con – Potentially unreliable, sometimes turned off due to noise. Filter/Fan air direction can paradoxically increase transmission by capturing (entraining) and blowing contaminated air towards susceptible people. Note that fan mixing alone (eg. back-to-back domestic heatpump) does not contribute to clean air changes per hour.
Use germicidal ultra-violet light (GUV), above head height – especially for locations where masks not worn.
- Can provide very high clean air changes equivalent, very cost effective, and in the case of FarUV, approach outdoor ‘safety’ condition. GUV systems are widely used in healthcare and airports and are considered safe with no direct UV exposure.
- Pro – Reliable, very effective and very cost effective, generally silent, no filters required, inactivates virus, kills bacteria in the air before transmission.
- Con – Specialist help required. Some (2 ACH) fresh air required.
Find and remove stagnant air
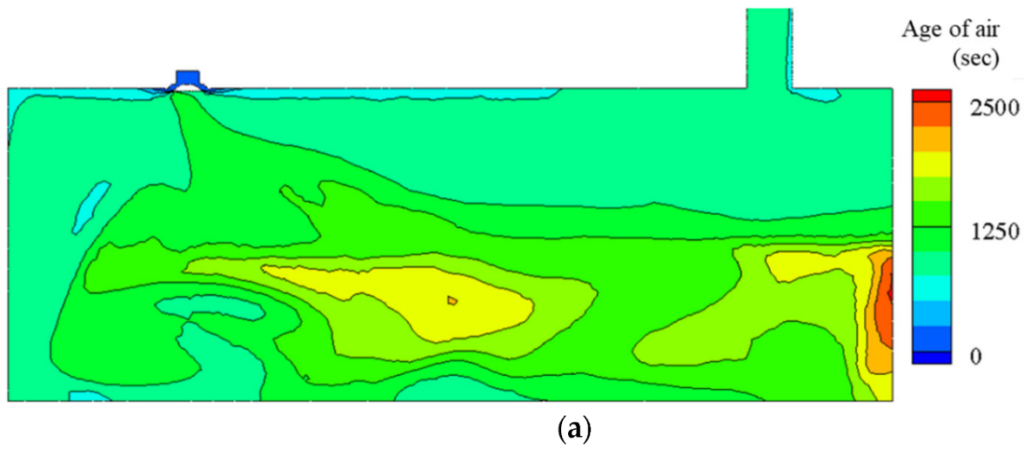
This room cross section with ceiling air supply (top left) and ceiling exhaust (top right) reveals the location of relatively stagnant air (in red) despite HVAC. Such areas of stagnant air will almost certainly be found (eg. by measuring CO2) even with correctly working HVAC.
What this implies is that HVAC designed to supply 6 air changes per hour may only be supplying 3 or 2 or less air changes to these areas with elevated CO2 levels. Extra air treatment eg. filtering (ideally HEPA), or fan/mixing will be required to level up these stagnant air zones.
Whichever methods are chosen, airflow should ideally be appropriate to achieve 600ppm CO2 or less over a workday (CDC USA and Education NZ both suggest 800ppm). Notice that this is not a guideline or a building standard but an ongoing performance requirement.
Match ventilation to room occupancy
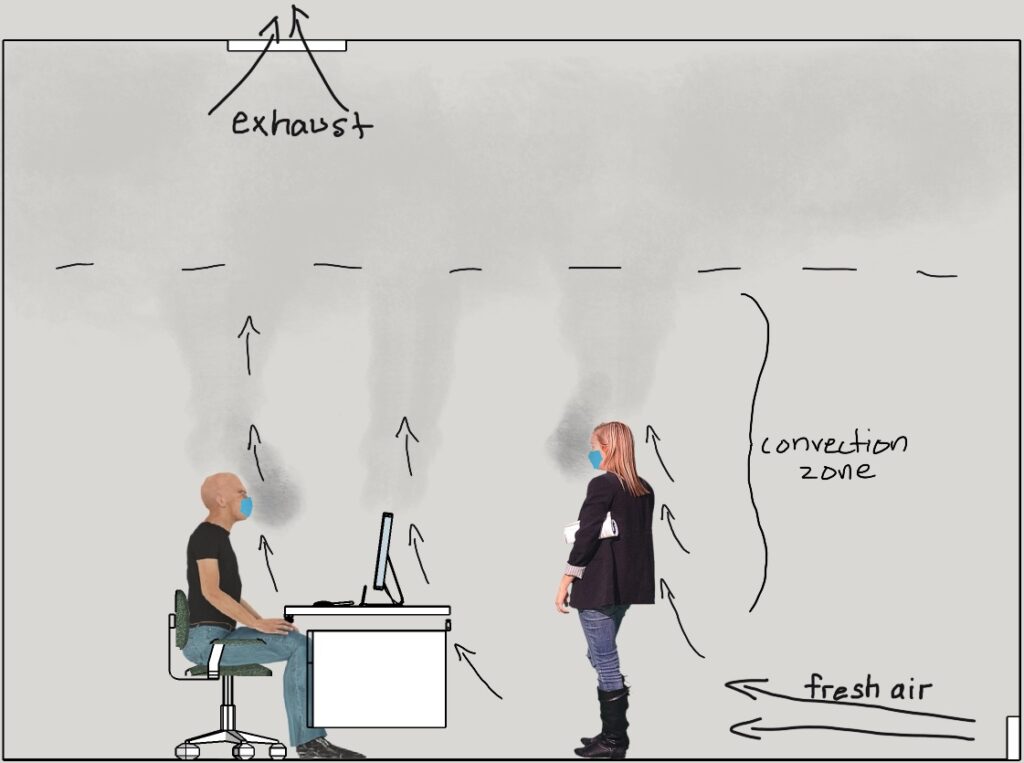
The scenario shown below shows too little ventilation causing the decline of room protection.
Rising warm air (stack effect convection) offers temporary room protection but the cloud of infective air gets lower, eventually filling the room. Inadequate ventilation allows virus clouds (and CO2) to build up in the room. As long as this imbalance continues, virus levels can increase.
Mask to avoid close range infection
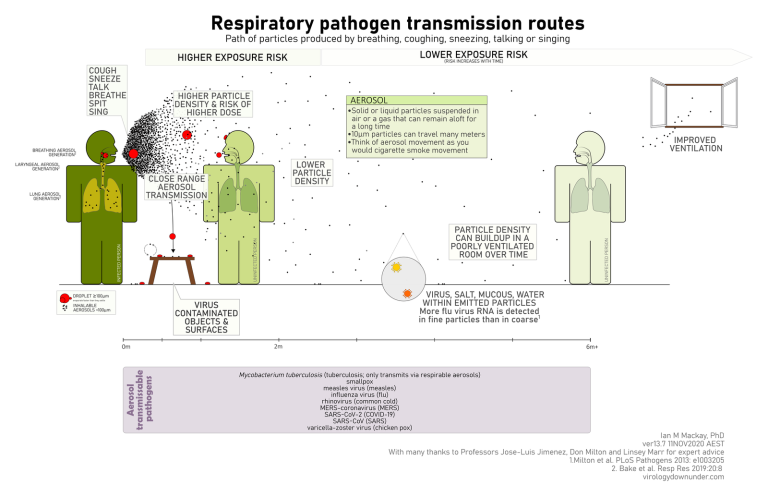
Figure 5. While transmission of SARS-CoV-2 is by an airborne route, the infectious dose at close range is higher than at a distance, but the viral load of virus-laden particles in a closed room can build up. The use of CO2 concentration is a helpful guide to identifying poor air exchange (“stale air”) in a room, but it won’t help you avoid close-range aerosol transmission and infection. Only a mask can help avoid that.
Ventilation, masking, distancing, filtering and UV disinfection all suppress transmission of virus and COVID-19.
N95 Masking nearly eliminates close-range aerosol transmission.
Masking reduces virus in the room.
Distancing is more effective when masks are worn.
Maximum room occupancy must fit within available ventilation.
Details of room size, occupancy, ventilation and risk implications of CO2 levels can be found in reference models such as ventilation and virus transmission analysis and at itsairborne.
Further reading: https://itsairborne.com/ – Joey Fox, HVAC specialist and Engineer, Charles Forsburgh on Stopping Pandemics.
Clean Air is Good Business.
